Search
- Page Path
- HOME > Search
- Clinical Study
- Insulin Secretion and Insulin Resistance Trajectories over 1 Year after Kidney Transplantation: A Multicenter Prospective Cohort Study
- Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Su Hyung Lee, Ja Young Jeon
- Endocrinol Metab. 2020;35(4):820-829. Published online November 18, 2020
- DOI: https://doi.org/10.3803/EnM.2020.743
- 4,944 View
- 119 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated the changing patterns of insulin secretion and resistance and risk factors contributing to the development of post-transplant diabetes mellitus (PTDM) in kidney recipients under tacrolimus-based immunosuppression regimen during 1 year after transplantation.
Methods
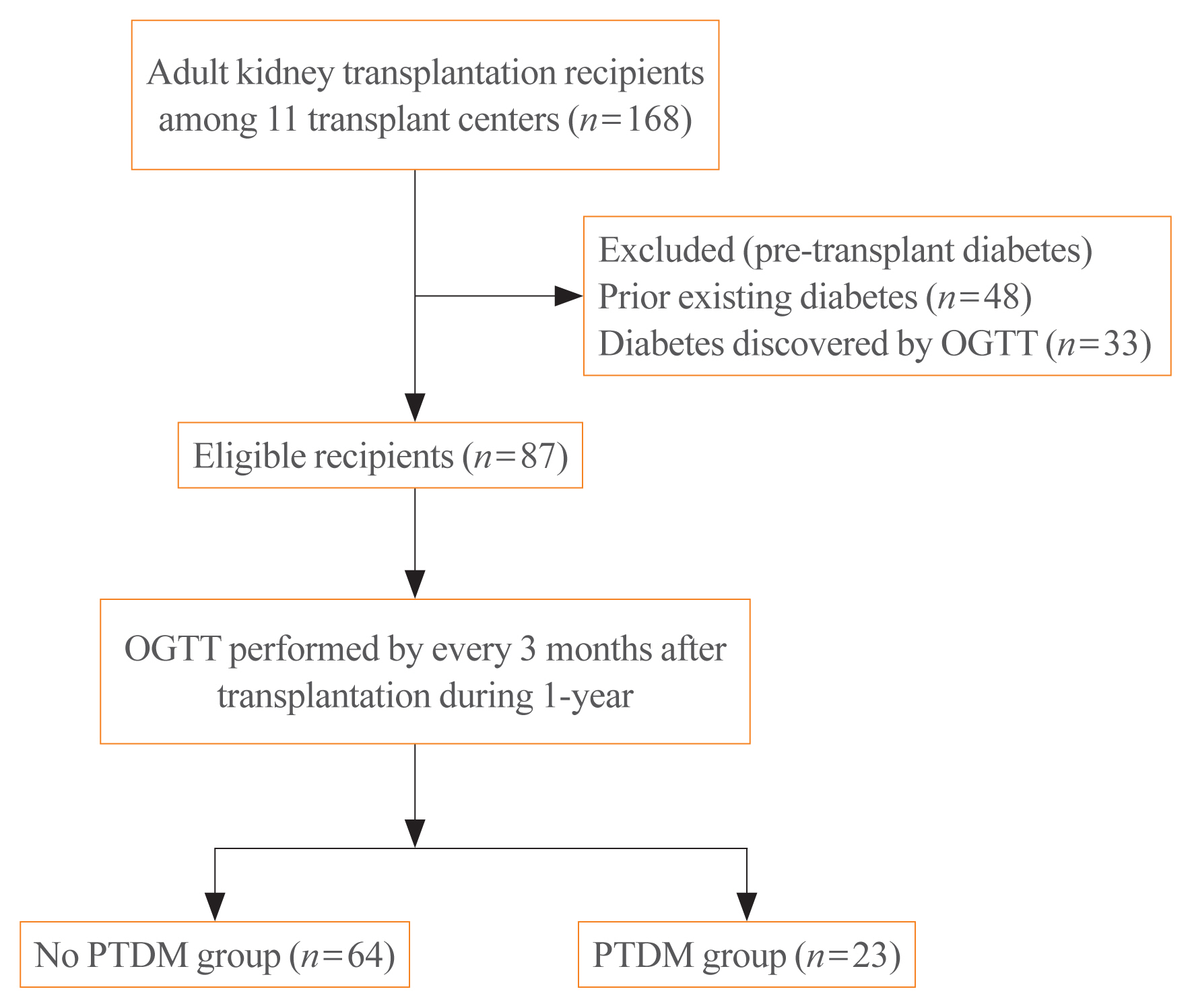
This was a multicenter prospective cohort study. Of the 168 subjects enrolled in this study, we analyzed a total 87 kidney transplant recipients without diabetes which was assessed by oral glucose tolerance test before transplantation. We evaluated the incidence of PTDM and followed up the index of insulin secretion (insulinogenic index [IGI]) and resistance (homeostatic model assessment for insulin resistance [HOMA-IR]) at 3, 6, 9 months, and 1 year after transplantation by oral glucose tolerance test and diabetes treatment. We also assessed the risk factors for incident PTDM.
Results
PTDM developed in 23 of 87 subjects (26.4%) during 1 year after transplantation. More than half of total PTDM (56.5%) occurred in the first 3 months after transplantation. During 1 year after transplantation, insulin resistance (HOMA-IR) was increased in both PTDM and no PTDM group. In no PTDM group, the increase in insulin secretory function to overcome insulin resistance was also observed. However, PTDM group showed no increase in insulin secretion function (IGI). Old age, status of prediabetes and episode of acute rejection were significantly associated with the development of PTDM.
Conclusion
In tacrolimus-based immunosuppressive drugs regimen, impaired insulin secretory function for reduced insulin sensitivity contributed to the development of PTDM than insulin resistance during 1 year after transplantation. -
Citations
Citations to this article as recorded by- Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Distúrbio do eixo hipotálamo-hipófise-gonadal e sua associação com resistência à insulina em receptores de transplante renal
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Hypothalamic-pituitary-gonadal axis disturbance and its association with insulin resistance in kidney transplant recipients
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Postoperative fasting plasma glucose and family history diabetes mellitus can predict post-transplantation diabetes mellitus in kidney transplant recipients
Le Wang, Jin Huang, Yajuan Li, Kewei Shi, Sai Gao, Wangcheng Zhao, Shanshan Zhang, Chenguang Ding, Wei Gao
Endocrine.2023; 81(1): 58. CrossRef - Changes in glucose metabolism among recipients with diabetes 1 year after kidney transplant: a multicenter 1-year prospective study
Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Hyung Joon Ahn, Su Hyung Lee, Ja Young Jeon
Frontiers in Endocrinology.2023;[Epub] CrossRef - Pretransplant evaluation and the risk of glucose metabolic alterations after renal transplantation: a prospective study
Arminda Fariña-Hernández, Domingo Marrero-Miranda, Estefania Perez-Carreño, Antonia De Vera-Gonzalez, Alejandra González, Cristian Acosta-Sorensen, Ana Elena Rodríguez-Rodríguez, Tatiana Collantes, Marta del Pino García, Ana Isabel Rodríguez-Muñoz, Carla
Nephrology Dialysis Transplantation.2022;[Epub] CrossRef
- Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis

- Clinical Study
- Effects of Dipeptidyl Peptidase-4 Inhibitors on Hyperglycemia and Blood Cyclosporine Levels in Renal Transplant Patients with Diabetes: A Pilot Study
- Jaehyun Bae, Min Jung Lee, Eun Yeong Choe, Chang Hee Jung, Hye Jin Wang, Myoung Soo Kim, Yu Seun Kim, Joong-Yeol Park, Eun Seok Kang
- Endocrinol Metab. 2016;31(1):161-167. Published online March 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.1.161
- 5,687 View
- 58 Download
- 21 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The use of dipeptidyl peptidase-4 (DPP-4) inhibitors is increasing among renal transplant patients with diabetes. However, the glucose-lowering efficacies of various DPP-4 inhibitors and their effects on blood cyclosporine levels have not been fully investigated. We compared the glucose-lowering efficacies of DPP 4 inhibitors and evaluate their effects on the blood levels of cyclosporine in renal transplant recipients with diabetes.
Methods Sixty-five renal allograft recipients who received treatment with DPP-4 inhibitors (vildagliptin, sitagliptin, or linagliptin) following kidney transplant were enrolled. The glucose-lowering efficacies of the DPP-4 inhibitors were compared according to the changes in the hemoglobin A1c (HbA1c) levels after 3 months of treatment. Changes in the trough levels of the cyclosporine were also assessed 2 months after treatment with each DPP-4 inhibitor.
Results HbA1c significantly decreased in the linagliptin group in comparison with other DPP-4 inhibitors (vildagliptin –0.38%±1.03%, sitagliptin –0.53%±0.95%, and linagliptin –1.40±1.34;
P =0.016). Cyclosporine trough levels were significantly increased in the sitagliptin group compared with vildagliptin group (30.62±81.70 ng/mL vs. –24.22±53.54 ng/mL,P =0.036). Cyclosporine trough levels were minimally changed in patients with linagliptin.Conclusion Linagliptin demonstrates superior glucose-lowering efficacy and minimal effect on cyclosporine trough levels in comparison with other DPP-4 inhibitors in kidney transplant patients with diabetes.
-
Citations
Citations to this article as recorded by- Diabetic Kidney Disease in Post-Kidney Transplant Patients
Ngoc-Yen T. Pham, Diego Cruz, Luis Madera-Marin, Raja Ravender, Pablo Garcia
Journal of Clinical Medicine.2024; 13(3): 793. CrossRef - International consensus on post-transplantation diabetes mellitus
Adnan Sharif, Harini Chakkera, Aiko P J de Vries, Kathrin Eller, Martina Guthoff, Maria C Haller, Mads Hornum, Espen Nordheim, Alexandra Kautzky-Willer, Michael Krebs, Aleksandra Kukla, Amelie Kurnikowski, Elisabeth Schwaiger, Nuria Montero, Julio Pascual
Nephrology Dialysis Transplantation.2024; 39(3): 531. CrossRef - Metabolic Disorders in Liver Transplant Recipients: The State of the Art
Filippo Gabrielli, Lucia Golfieri, Fabio Nascimbeni, Pietro Andreone, Stefano Gitto
Journal of Clinical Medicine.2024; 13(4): 1014. CrossRef - Diabetic Kidney Disease in Post-Transplant Diabetes Mellitus: Causes, Treatment and Outcomes
Lee-Moay Lim, Jer-Ming Chang, Hung-Tien Kuo
Biomedicines.2023; 11(2): 470. CrossRef - Sweet and simple as syrup: A review and guidance for use of novel antihyperglycemic agents for post‐transplant diabetes mellitus and type 2 diabetes mellitus after kidney transplantation
S. Elise Lawrence, Mary Moss Chandran, Jeong M. Park, Helen Sweiss, Thomas Jensen, Palak Choksi, Barrett Crowther
Clinical Transplantation.2023;[Epub] CrossRef - Interventions Against Posttransplantation Diabetes: A Scientific Rationale for Treatment Hierarchy Based on Literature Review
Adnan Sharif
Transplantation.2022; 106(12): 2301. CrossRef - Dipeptidyl Peptidase-4 Inhibitor Decreases Allograft Vasculopathy Via Regulating the Functions of Endothelial Progenitor Cells in Normoglycemic Rats
Feng-Yen Lin, Chun-Min Shih, Chun-Yao Huang, Yi-Tin Tsai, Shih-Hurng Loh, Chi-Yuan Li, Cheng-Yen Lin, Yi-Wen Lin, Chien-Sung Tsai
Cardiovascular Drugs and Therapy.2021; 35(6): 1111. CrossRef - Review of Newer Antidiabetic Agents for Diabetes Management in Kidney Transplant Recipients
Sonya Anderson, Laura Cotiguala, Sarah Tischer, Jeong Mi Park, Katie McMurry
Annals of Pharmacotherapy.2021; 55(4): 496. CrossRef - Incretin based therapies and SGLT-2 inhibitors in kidney transplant recipients with diabetes: A systematic review and meta-analysis
Dora Oikonomaki, Evangelia Dounousi, Anila Duni, Stefanos Roumeliotis, Vassilios Liakopoulos
Diabetes Research and Clinical Practice.2021; 172: 108604. CrossRef - CD161a-positive natural killer (NK) cells and α-smooth muscle actin-positive myofibroblasts were upregulated by extrarenal DPP4 in a rat model of acute renal rejection
Franziska Schmid, Christina Mayer, Maike Büttner-Herold, Stephan von Hörsten, Kerstin Amann, Christoph Daniel
Diabetes Research and Clinical Practice.2021; 173: 108691. CrossRef - Current Pharmacological Intervention and Medical Management for Diabetic Kidney Transplant Recipients
Theerawut Klangjareonchai, Natsuki Eguchi, Ekamol Tantisattamo, Antoney J. Ferrey, Uttam Reddy, Donald C. Dafoe, Hirohito Ichii
Pharmaceutics.2021; 13(3): 413. CrossRef - Recent advances in new-onset diabetes mellitus after kidney transplantation
Tess Montada-Atin, G V Ramesh Prasad
World Journal of Diabetes.2021; 12(5): 541. CrossRef - Safety and Efficacy of Long-Term Administration of Dipeptidyl peptidase IV Inhibitors in Patients With New Onset Diabetes After Kidney Transplant
Adamantia Mpratsiakou, Marios Papasotiriou, Theodoros Ntrinias, Konstantinos Tsiotsios, Evangelos Papachristou, Dimitrios S. Goumenos
Experimental and Clinical Transplantation.2021; 19(5): 411. CrossRef - Medical management of metabolic and cardiovascular complications after liver transplantation
Chiara Becchetti, Melisa Dirchwolf, Vanessa Banz, Jean-François Dufour
World Journal of Gastroenterology.2020; 26(18): 2138. CrossRef - Efficacy and Safety of Dipeptidyl Peptidase-4 Inhibitors in Kidney Transplant Recipients with Post-transplant Diabetes Mellitus (PTDM)- a Systematic Review and Meta-Analysis
Tarek Samy Abdelaziz, Ahmed Yamany Ali, Moataz Fatthy
Current Diabetes Reviews.2020; 16(6): 580. CrossRef - NAFLD and liver transplantation: Disease burden, current management and future challenges
Patrizia Burra, Chiara Becchetti, Giacomo Germani
JHEP Reports.2020; 2(6): 100192. CrossRef - Linagliptin plus insulin for hyperglycemia immediately after renal transplantation: A comparative study
Rodolfo Guardado-Mendoza, David Cázares-Sánchez, María Lola Evia-Viscarra, Lilia M. Jiménez-Ceja, Edgar G. Durán-Pérez, Alberto Aguilar-García
Diabetes Research and Clinical Practice.2019; 156: 107864. CrossRef - Post-Liver Transplantation Diabetes Mellitus: A Review of Relevance and Approach to Treatment
Maria J. Peláez-Jaramillo, Allison A. Cárdenas-Mojica, Paula V. Gaete, Carlos O. Mendivil
Diabetes Therapy.2018; 9(2): 521. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Drug–drug interactions between immunosuppressants and antidiabetic drugs in the treatment of post-transplant diabetes mellitus
Thomas Vanhove, Quinten Remijsen, Dirk Kuypers, Pieter Gillard
Transplantation Reviews.2017; 31(2): 69. CrossRef - Risk assessment and management of post-transplant diabetes mellitus
Eugene Han, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Metabolism.2016; 65(10): 1559. CrossRef
- Diabetic Kidney Disease in Post-Kidney Transplant Patients

- Retraction: Contributing Factors to Different Natural Courses of Posttansplantation Diabetes Mellitus in Renal Allograft Recipients.
- Kyu Yeon Hur, Myoung Soo Kim, Jae Hyun Nam, Eun Seok Kang, Hyun Joo Lee, So Hun Kim, Bong Soo Cha, Chul Woo Ahn, Soon Il Kim, Yu Seun Kim, Hyun Chul Lee
- J Korean Endocr Soc. 2007;22(6):479. Published online December 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.6.479
- 1,522 View
- 21 Download

- Contributing Factors to Different Natural Courses of Posttansplantation Diabetes Mellitus in Renal Allograft Recipients.
- Kyu Yeon Hur, Myoung Soo Kim, Jae Hyun Nam, Eun Seok Kang, Hyun Joo Lee, So Hun Kim, Bong Soo Cha, Chul Woo Ahn, Soon Il Kim, Yu Seun Kim, Hyun Chul Lee
- J Korean Endocr Soc. 2006;21(5):373-381. Published online October 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.5.373
- 2,000 View
- 22 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
New onset diabetes is a major complication after kidney transplantation. However, the natural course of posttransplantation diabetes mellitus (PTDM) remains unclear. The aim of this study was to demonstrate the detailed natural courses of PTDM according to the onset and persistency of hyperglycemia, and to investigate risk factors for development of different courses of PTDM in renal allograft recipients. METHODS: A total of 77 renal allograft recipients without previously known diabetes were enrolled and performed a serial 75 g oral glucose tolerance test at 0, 1, and 7 years after kidney transplantation. Patients were classified according to the onset and persistency of PTDM: early PTMD (E-PTDM), late PTDM (L-PTDM), persistent PTDM (P-PTDM), transient PTMD (T-PTDM), and non-PTDN (N-PTDM). RESULTS: The incidence of each group was as follows: E-PTDM, 39%; L-PTDM, 11.7%; P-PTDM, 23.4% T-PTDM, 15.6%; N-PTDM, 49.3%. Tacrolimus and female gender were associated with the development of E-PTDM. Among E-PTDM, age at transplantation was a high risk factor for the development of P-PTDM. Higher BMI at year1 was associated with the development of L-PTDM. CONCLUSION: Different risk factors were associated with various natural courses of PTDM. Since old age and female gender are not modifiable risk factors, it may be important to modify immunosuppressive therapy regimens for the prevention of E-PTDM and control of body weight for L-PTDM. -
Citations
Citations to this article as recorded by- Efficacy and Safety of Gemigliptin in Post-Transplant Patients With Type 2 Diabetes Mellitus
Jaehyun Bae, Youjin Kim, Yongin Cho, Minyoung Lee, Ji-Yeon Lee, Yong-ho Lee, Byung-Wan Lee, Bong-Soo Cha, Dong Jin Joo, Kyu Ha Huh, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Transplantation Proceedings.2019; 51(10): 3444. CrossRef - Post-transplantation Diabetes Mellitus
Kun-Ho Yoon
Journal of Korean Endocrine Society.2006; 21(5): 370. CrossRef
- Efficacy and Safety of Gemigliptin in Post-Transplant Patients With Type 2 Diabetes Mellitus


 KES
KES

 First
First Prev
Prev



